Research Summaries
Why was the study done?
A high proportion of serving Royal Canadian Mounted Police (RCMP) report having symptoms of mental health disorders such as Posttraumatic Stress Disorder (PTSD) and Major Depressive Disorder (MDD), with half screening positive for one or more mental health disorders.
In the past, mental health challenges have often been attributed to insufficient mental health screening of recruits, despite the mental health of Cadets entering the RCMP Cadet Training Program (CTP) being unknown. The current study was designed to provide an initial estimate of Cadet mental health when starting the CTP.
What was done in the study?
The current research is part of a larger RCMP Study designed to develop, deploy, and assess the impact of a system for ongoing annual, monthly, and daily evidence-based assessments; and enhancing the RCMP CTP with evidence-based skills to help protect members from experiencing Posttraumatic Stress Injuries (PTSI). A research summary of the previously published Study Protocol can be read here.
Participants were RCMP Cadets starting the 26-week CTP and voluntary participation was invited as part of standard training. The current study focuses on data collected between May 2019 and October 2021, and included: web-delivered surveys assessing self-reported mental health symptoms, completed by 772 participants; and clinical interviews assessing current and past mental health, completed by 736 participants. A total of 707 participants completed both the surveys and the interviews.
What did we find out?
There were few statistically significant differences on mental disorder symptoms across demographic categories. Based on self-report measures, female Cadets were more likely to screen positive for current MDD, Generalized Anxiety Disorder (GAD), and Social Anxiety Disorder (SAD). Based on clinical interviews, females were less likely than males to meet criteria for Alcohol Use Disorder (AUD).
Comparisons with the General Public:
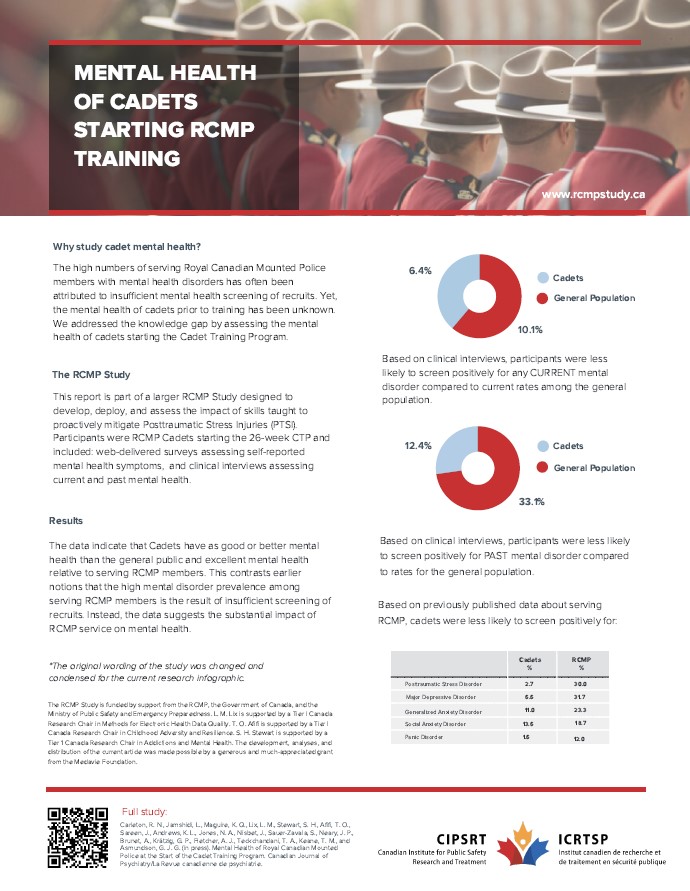
Comparisons must be interpreted with caution due to differing assessment models and the inability to control for sociodemographic factors. Participants were more likely to self-report symptoms of GAD in the past two weeks than the general population, possibly because of temporary stressors related to starting the CTP. Based on clinical interviews, participants were actually less likely to screen positively for any current mental disorder (6.3%) than the general public (10.1%). Compared to the general population (33.1%), participants were also less likely to have difficulties with a past mental health disorder based on results from self-report (3.9%) and clinical interviews (12.4%).
Comparisons with Serving RCMP:
The data were also compared to previously published data on RCMP members who had an average of 17.42 years of service. Overall, study participants self-reported fewer mental disorders symptoms and positive screens than serving RCMP members.
Where do we go from here?
The current results help address a gap in the existing research by providing initial evidence about the mental health of Cadets beginning the CTP. The data indicates that Cadets had lower prevalence of anxiety-, mood-, and trauma-related mental disorder symptoms than the general public, and much lower than serving RCMP members. The results contrast notion that more rigorous mental health screening of Cadets would reduce the prevalence of mental health disorders among serving RCMP. The results underscore the importance of research focusing on Cadets starting their training and suggest that ongoing mental health supports are necessary to mitigate the substantial impact of service on RCMP mental health.
The results help to continue advancing Canada’s first-ever National Action Plan on Post-Traumatic Stress Injuries, including additional investment to support the health and well-being of first responders and other public safety personnel.
The RCMP Study is funded by support from the RCMP, the Government of Canada, and the Ministry of Public Safety and Emergency Preparedness. L. M. Lix is supported by a Tier I Canada Research Chair in Methods for Electronic Health Data Quality. T. O. Afifi is supported by a Tier I Canada Research Chair in Childhood Adversity and Resilience. S. H. Stewart is supported by a Tier 1 Canada Research Chair in Addictions and Mental Health. The development, analyses, and distribution of the current article was made possible by a generous and much-appreciated grant from the Medavie Foundation.
Original study
Carleton, R. N., Jamshidi, L., Maguire, K. Q., Lix, L. M., Stewart, S. H., Afifi, T. O., Sareen, J., Andrews, K. L., Jones, N. A., Nisbet, J., Sauer-Zavala, S., Neary, J. P., Brunet, A., Krätzig, G. P., Fletcher, A. J., Teckchandani, T. A., Keane, T. M., and Asmundson, G. J. G. (in press). Mental Health of Royal Canadian Mounted Police at the Start of the Cadet Training Program. Canadian Journal of Psychiatry/La Revue canadienne de psychiatrie.
Prepared by K. Vincent